Delicate women’s health issues often go unnoticed because they are difficult to talk about openly. One such situation is a bladder-vaginal fistula, a condition in which an abnormal connection forms between the bladder and the vagina, causing constant urine leakage and noticeable physical and emotional discomfort. Many women get used to the symptoms, are embarrassed to discuss them, and put off seeing a doctor, even though modern medicine has effective treatments available. This article is designed to calmly and clearly explain the nature of the problem and help you decide to seek medical help in a timely manner.
What is a bladder-vaginal fistula in simple terms
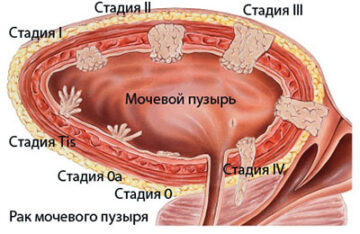
A bladder-vaginal fistula occurs when the tissues between the bladder and the vagina, which should normally be completely separated, are damaged. As a result, a small opening forms through which urine begins to enter the vagina outside of the natural process of urination. This does not happen because the body wants it to, or because of “weak muscles”, but because of a structural defect that disrupts the normal anatomy and functioning of the organs.
It is important to understand that a vaginal fistula is not a form of urinary incontinence or a manifestation of ordinary inflammation or infection. These conditions may have similar symptoms, but the mechanism of their occurrence is fundamentally different. A bladder-vaginal fistula always requires medical evaluation because without accurate diagnosis and treatment, the problem persists and may worsen over time. A calm and timely approach allows you to find an effective solution and regain control of the situation.
Why does a bladder-vaginal fistula occur?
In most cases, a vaginal fistula does not form spontaneously, but as a result of certain medical situations in which the tissues of the small pelvis are subjected to significant stress or damage. Most often, the problem arises some time after interventions or events that disrupt the integrity of the tissues between organs. Symptoms may not appear immediately, making it difficult to establish a link between cause and effect and forcing women to search for an explanation for their condition for a long time. The most common causes of vaginal fistula include:
- surgery on the pelvic organs, including gynaecological and urological surgery;
- difficult or traumatic childbirth accompanied by tissue tears;
- cancer treatment;
- mechanical trauma and the consequences of inflammatory processes that interfere with healing.
It is important to emphasise that the appearance of this condition is not related to mistakes or “fault” on the part of the woman herself. This problem is most often a medical complication that requires the attention of a specialist and competent treatment. Understanding the causes helps to notice changes in well-being in a timely manner and to discuss symptoms that should raise alarm bells and prompt a visit to the doctor.
What symptoms should raise alarm bells
The symptoms that accompany a bladder-vaginal fistula do not always appear suddenly. More often, they develop gradually, which is why a woman may not associate changes in her well-being with the disease for a long time. It seems that the problem is “tolerable” or temporary, and over time, one simply gets used to it, although this condition is not normal and requires medical evaluation. Here are the most common signs that may indicate a problem:
- constant or periodic leakage of urine outside of urination;
- a feeling of wetness in the intimate area and a persistent unpleasant odour;
- skin irritation, redness and discomfort;
- frequent inflammation of the urinary tract or vagina;
- feelings of embarrassment and psychological discomfort in everyday and intimate life.
Even if the symptoms listed are mild or do not occur every day, they should not be ignored. If you experience these symptoms, it is important to see a specialist and have yourself checked, as vaginal fistulas are treatable, especially if diagnosed early.
The dangers of ignoring the problem
Ignoring delicate symptoms is often associated with the hope that the condition will stabilise on its own. However, a bladder-vaginal fistula is a problem that usually does not go away without medical attention. Constant contact of tissues with urine gradually affects overall well-being, reduces comfort and can cause new complaints that go beyond the initial sensations. Over time, the problem can lead to the following consequences:
- Inflammatory processes in the bladder and vagina.
- Painful sensations and irritation of the mucous membranes.
- Deterioration of intimate hygiene and a constant feeling of discomfort.
- A decrease in quality of life, sleep disturbances, and sexual discomfort.
- Gradual enlargement of the fistula, which complicates further treatment.
It is important to note that postponing a visit to the doctor does not solve the problem, but only makes the road to recovery longer. Timely treatment allows for an early assessment of the condition and selection of the optimal treatment for bladder-vaginal fistula without unnecessary complications.
How doctors diagnose bladder-vaginal fistula
The diagnosis begins with a calm conversation and a careful examination. The doctor clarifies the complaints, specific symptoms, previous operations, childbirth and other medical circumstances that could have affected the condition of the tissues. At this stage, the specialist may already suspect a vaginal fistula and determine what actions are necessary, without unnecessary procedures and overloading the patient.
To clarify the diagnosis, additional tests may be prescribed: laboratory tests, special tests with dyes, ultrasound, and other imaging methods. Their purpose is to accurately determine the size and location of the fistula, which is important for choosing a treatment plan. The selection of tests is always individual, and many procedures are comfortable, performed in a calm environment and under the supervision of a specialist, taking into account the woman’s well-being and emotional state.
Modern treatment methods
The approach to treatment is always selected individually, because bladder-vaginal fistulas can vary in size, location and causes. The doctor assesses the general condition, how long the problem has existed and the impact of the symptoms on the quality of life. In some situations, observation and supportive therapy aimed at reducing inflammation and creating conditions for tissue healing may be possible. This option is only considered when there are clear medical indications and under the regular supervision of a specialist. Depending on the clinical picture, the following treatment methods may be used:
- A wait-and-see approach with medication support for minor defects.
- Planned surgical treatment aimed at closing the fistula and restoring anatomy.
- Postoperative monitoring and rehabilitation under the supervision of a doctor.
The Avicenna Clinic uses modern and comfortable approaches to treatment, with an emphasis on accuracy and safety. One of the most effective methods is laparoscopic plastic surgery, which allows for careful tissue restoration with minimal trauma. After the procedure, the woman gradually returns to her normal lifestyle, and the rehabilitation period helps to restore physical comfort, self-confidence and a sense of control over her own body.
When to see a doctor
It is worth consulting a doctor if you experience constant urine leakage, an increase in unpleasant odour, pain, fever or any deterioration in your well-being. Special attention should be paid to situations where such symptoms occur after childbirth, surgery, or treatment of the pelvic organs. Even if the symptoms seem mild, a vaginal fistula can develop gradually, so early consultation helps to accurately determine the cause and avoid complications.
At our Avicenna clinic, consultations take place in a calm and supportive atmosphere, where patient safety and comfort are our top priorities. Consultations allow us not only to make a diagnosis, but also to develop a clear plan of further action aimed at restoring quality of life. You can learn more about the options and approaches in the “Fistula Treatment” section, which describes the modern methods of care and individual approach to each woman that our specialists use.
Psychological aspects and support
When faced with this problem, women often experience shame, anxiety and a feeling of isolation. A bladder-vaginal fistula affects not only physical health, but also emotional well-being, impacting self-esteem and self-confidence. These feelings are natural and understandable, but it is important to remember that you do not have to deal with them alone. Support and professional help can gradually restore a sense of control and calm.
Seeing a doctor is not a sign of weakness, but a conscious step towards solving the problem. An open conversation with your partner and loved ones can help reduce internal tension and feelings of loneliness. After treatment for a vaginal fistula, most women return to their normal routine, regaining comfort, confidence and the ability to live without constant restrictions.
Conclusion
A bladder-vaginal fistula is a delicate but entirely treatable medical condition in which timely assistance plays a key role. Early diagnosis and properly selected treatment can prevent complications and restore physical comfort and quality of life. If you experience any alarming symptoms or changes in your well-being, do not delay in seeing a specialist — paying close attention to your health will help you regain your confidence and peace of mind.
FAQ
- Can a bladder-vaginal fistula be cured without surgery?
In some cases, if the fistula is small, your doctor may recommend observation and supportive therapy. However, more often than not, the problem requires surgical treatment. The decision is made on an individual basis after diagnosis.
- How does a vaginal fistula differ from urinary incontinence?
A vaginal fistula is an anatomical connection between organs through which urine is constantly or periodically discharged. Urinary incontinence is associated with a malfunction of the muscles and sphincters and requires a different approach to treatment.
- Is it dangerous to delay treatment for a bladder-vaginal fistula?
Yes, postponing treatment can lead to inflammation and enlargement of the defect. Early diagnosis reduces the risk of complications and makes treatment less complicated.
- Can I lead a normal life after treatment?
After successful treatment and rehabilitation, women return to their normal lives, including work and personal relationships. The right approach helps restore comfort and confidence.