Based on materials of 21 European Vascular Course
(Maastricht the Netherlands, 5-7 March 2017)
In Maastricht, the Kingdom of the Netherlands, the annual European Vascular Course (EVC) was held on March 5-7, 2017, which traditionally summarizes the results of the use of modern methods and technologies in vascular surgery, trends, trends and perspectives in this area are formed.
The program has traditionally consisted of three main sections: the arterial section, the venous section and the vascular access section (Vascular Access Course).
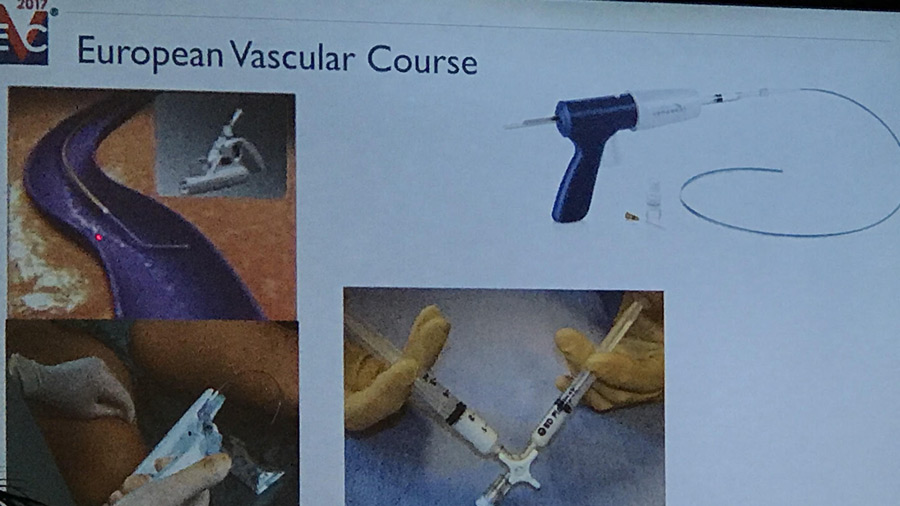
A distinctive feature of EVC is that along with the extensive theoretical part presented both by program reports and numerous materials about its own results, great attention is paid to the possibility of improving practical skills, mastering modern technologies during workshops, which are conducted by the world’s leading manufacturers (Fig. 1)
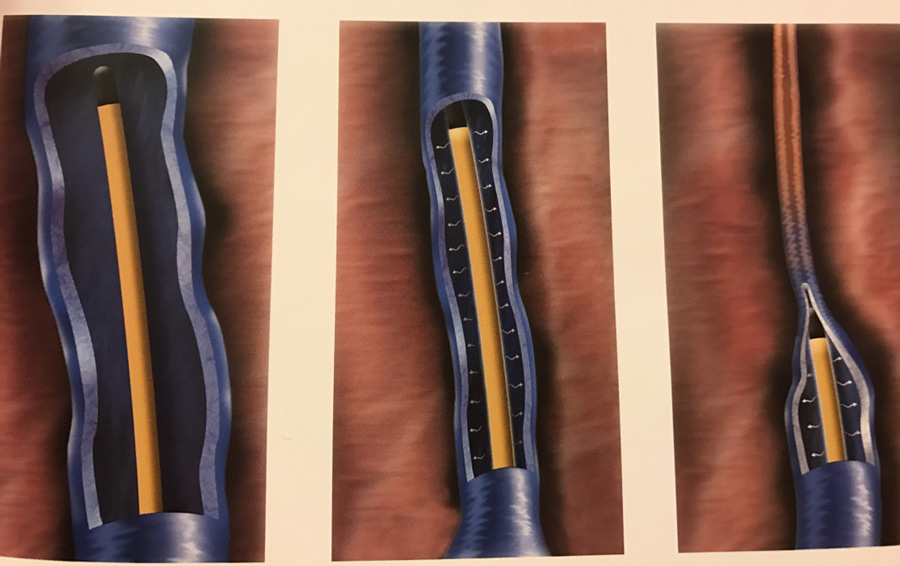
Attention is drawn to the widespread introduction of 3-D technologies, which are used both for reports and directly at Workshops, which raises the perception of information to a different quality level (Fig. 2.3)
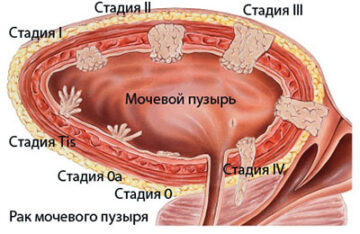
Let’s get back to the section of phlebology. Why there are diseases of veins?
As a result of various factors and causes, known for a long time, such as heredity, overweight, prolonged static loads, pregnancy, etc., the main cause of chronic venous disease is stagnation, hypertension (high blood pressure) in certain areas of the venous system lower extremities, as a result of which telangiectasias are formed, varicose transformation of the subcutaneous veins.
What methods of treatment of chronic venous disease are applied today?
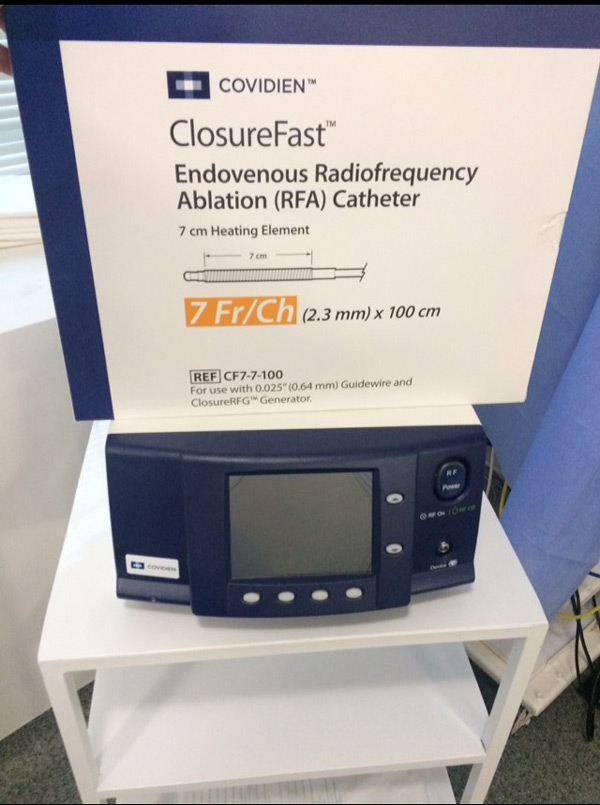
The basis of modern phlebology for the treatment of venous diseases is intravascular interventions, which include laser technology, radiofrequency ablation, foam form of sclerotherapy, biological glue (Fig. 4, 5). These types of surgical interventions optimally meet the requirements of aesthetic phlebology — «no incisions — no scars».
The basis of modern phlebology for the treatment of venous diseases is intravascular interventions, which include laser technology, radiofrequency ablation, foam form of sclerotherapy, biological glue (Fig. 4, 5). These types of surgical interventions optimally meet the requirements of aesthetic phlebology — «no incisions — no scars».
The criterion of success is an understanding of the underlying processes of the pathogenesis of the development of venous disease and the possession of ultrasound technology.
It is of fundamental importance to perform a radical intervention in the early stages, when it is sufficient to eliminate the cause by intravascular intervention from one! the only puncture. In Europe, more than 70% of surgical interventions are performed in this way. In the case of a pronounced varicose veins, the main stage of the operation must be supplemented with either a frothy form of the spirotherapy or a miniflebectomy, the latter is certainly aesthetically loses, as depending on the severity of the varicose is performed from 3-5 to 12-15, sometimes 20 additional punctures. Given that varicose veins are a continuously progressive disease, there are no conservative treatments and reverse development of the process. At the best, we can talk about «slowing down» the process. Hence, the conclusion — early treatment, allows you to solve phlebological problems with the maximum cosmetic effect.
What are the main advantages of intravascular interventions?
Intravascular interventions performed on time and on indications are accompanied by maximum cosmetic effect, in fact the entire operation can be performed from a single puncture 2-3 mm in size, comfort during surgery and most importantly, after the compression knitwear is worn on the operating table, the patient independently rises from the operating table, for 25-30 minutes walks in the clinic, often for this are used treadmills, after which he leaves home (he can drive himself) with a feeling that im all good.
It is very significant that patients who require intervention consistently on both lower extremities are asked when it is possible to register for the next operation literally in the operating room as soon as they rise from the operating table.
I want to emphasize the maximally high effectiveness of minimally invasive intravascular interventions, the statement is absolutely justified — without loss of radicalism, i. e. the effectiveness of the methods is 97-98%, the number of relapses is no more than 2-3%.
What do you consider to be the most progressive technique? Laser or radiofrequency ablation?
In my work I use endovenous radio frequency ablation (RFO), which in my understanding is the «gold standard» of endovenous surgery, but I want to add that everything depends on the surgeon’s experience and skills, there are worthy results for colleagues who perform laser obliteration.
However, today the most progressive and promising technique is the use of biological glue (biocides).
Biological glue, what is it and what are its advantages?
A distinctive feature of biological glue is that the recovery occurs directly on the operating table, in contrast to laser and radiofrequency obliteration, where it is necessary to follow recommendations for a certain time, for example daily walking for at least 30-60 minutes, including immediately after the operation, wearing compression knitwear up to 3 weeks, etc., the need to perform tumescent anesthesia during surgery.
The use of biological glue can be recommended, both at the request of the patient himself and for medical reasons, for example a polyvalent allergy to anesthetics, the inability to wear compression knitwear, a sedentary lifestyle. Along with these advantages, it must be emphasized that the method of using biocides requires the highest level of training from a surgeon, a great experience in conducting intravascular interventions, filigree possession of ultrasound diagnostics, otherwise the technique has serious complications.
The leader in the world market of endovenous bioglues is VenaSeal TM (Medtronic), EVOLO Biolas and technology — Endovenous glue ablation were also presented at EVC 2017, these technologies are currently certified in Ukraine, and I think that in the near future will be available for our patients.
In the EVC 2017 review, I want to mention the work of the International Compression Club (ICC), whose numerous reports have presented a large number of studies, with a maximum degree of certainty, up to the cellular level, proving the appropriateness and effectiveness of properly selected compression therapy literally with the entire spectrum of phlebological pathology.
What does correct compression mean?
The key issues in the selection of compression therapy are two main parameters: the choice of the manufacturer and the individual selection of the product. The main requirement for the manufacturer is a check in the factory of the degree of compression, as well as a guarantee for the continued compression in conditions of proper operation for a long time. Individual selection of compression knitwear is based on two main parameters: the first definition of the degree of compression, depending on the severity of the underlying and accompanying pathology and is measured in compression classes and size selection for each patient.
Currently, there are automated technologies for the selection of compression knitwear, characterized by an individual selection of maximum accuracy (Figure 9). Taking into account that the compression ratio is measured in mm Hg, and the oscillations between classes are 5-10 mm Hg, even an insignificant error can level the expected result.
I advise you to prefer specialized shops of well-known brands that, on the one hand, during the production process, check, perform individual measurement and selection of knitwear, explain how to properly use and «look after», and give a guarantee on the safety of the compression degree in a period of at least 6 months. I can only caution against purchases through the online store or in the nearest (to home) pharmacy, where the choice is limited and the commercial result comes to the fore
What kind of knitwear do you use in your work?
I would like to avoid commercial names I will only say that in my work I use the compression jersey of German manufacturers who possess all of these characteristics. By the way, there are 3 of them in Germany, which is interesting, in Germany they all have the same price
It is necessary to emphasize that modern technologies for making compression knitwear have far stepped not only in the medical, but also in the aesthetic direction, leading European manufacturers are knitted as 7 different, already traditional colors, and quite original prints (Figure 10)
Thus, modern phlebology has a wide range of possibilities for solving all the problems with chronic disease of the veins of the lower extremities, using individually substantiated complex modern techniques and achieving maximum cosmetic effect: no incisions — no scars
Source: Journal of Les Nouvelles Esthetiques Ukraine (No. 3/2017)